Without doubt being very old is the single biggest risk factor for Covid 19, but not just age on its own. Inflammaging or high levels of chronic inflammation as a person ages is the driving force behind susceptibility to Covid 19. Even though we see young people dying 99% of deaths are related to chronic inflammation.
A recent study found the infection fatality rate (IFR -that is how many people actually die once they are infected) for COVID-19 is close to zero for younger adults but rises exponentially with age, reaching about 0.3% for ages 50-59, 1.3% for ages 60-69, 4% for ages 70-79, 10% for ages 80-89. In fact studies have suggested the infection fatality rate for children is around 0.03% around 1000 times less than people in their 80’s.
When younger people die and it always seems to get major media attention it has almost exclusively linked with chronic inflammation and major diseased states and at a rate no higher than the annual influenza incidence. The 5 most common modifiable risk factors for Covid 19 are hypertension, diabetes, elevated blood sugar (independent of diabetes), obesity and smoking. Many other risk factors have been identified including the use of proton pump inhibitors (PPI’s) for reflux. All of these conditions are linked through malnutrition, inflammation and metabolic conditions. In the UK Two-thirds of people who have fallen seriously ill with COVID-19 were overweight or obese and 99% of deaths in Italy have been in patients with pre-existing conditions, such as hypertension, diabetes and heart disease.
As of May 30, 2020, among COVID-19 cases, the most common underlying health conditions were cardiovascular disease (32%), diabetes (30%), and chronic lung disease (18%). Hospitalisations were six times higher among patients with a reported underlying condition (45.4%) than those without reported underlying conditions (7.6%). Deaths were 12 times higher among patients with reported underlying conditions (19.5%) compared to those without reported underlying conditions (1.6%).
In one Systematic Review and Meta-Analysis including 14 studies with 29,909 COVID-19 infected patients and 1445 cases of death reported Older age (≥65 years old), male gender, hypertension, CVDs, diabetes, chronic obstructive pulmonary disease and malignancies were associated with greater risk of death from COVID-19 infection.
Interestingly, all these risk factors predispose people to increased risks from every type of viral infection including respiratory viruses and influenza at much the same rates as those identified above with the exception of the elderly. So what is it about the extremely old?
The real factor in all these deaths is chronic low-grade systemic inflammation that accompanies aging “inflammaging”. Inflammaging is linked to various age-related lifestyle diseases such as cardiovascular disease, cancer, neurodegenerative diseases, chronic obstructive pulmonary disease, diabetes, and rheumatoid arthritis.
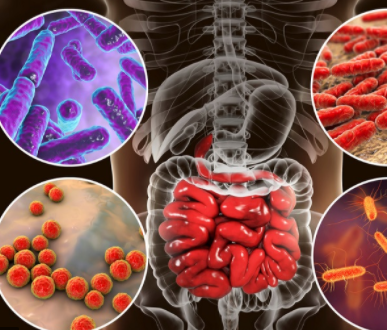
Characteristics of inflammaging also include an ageing gut microbiome linked to increasingly poor nutrition. The elderly, especially in age care facilities where most of the deaths occur, are renowned for their low nutritional quality food. As a result the gut microbiota diversity is decreased in old age as is the immune and health benefits related to the gut microbiome.
An apparent age-related gut microbiota imbalance has been underscored in the last years, featured by an altered microbial diversity, a lower abundance of probiotic strains (e.g. Bifidobacteria) and a reduced number of species producing butyrate, a short chain fatty acid (SCFA) that plays important metabolic functions and has a major role in maintaining the integrity of intestinal epithelium. Notably, age-related alterations in gut microbiota composition and function deeply impairs local (gut) and distal immunity. For instance, it is known that the systemic priming of inflammasomes (a mechanism closely regulated by gut microbiota) increases with age. Gut microbiota dysbiosis has been also associated with a diversity of age-related cardiac and vascular disorders, including hypertension, heart failure, myocardial infarction, stroke and coronary artery disease, not to mention susceptibility to other viral infections.
So what is the answer to this Covid situation?
Simply it all comes back to the basic common sense approach to good nutrition throughout our lives and protecting our elderly through high dose antioxidant, antiinflammatory and gut healing nutrients. But more on this later.
Major sources:
Microbiota Modulating Nutritional Approaches to Countering the Effects of Viral Respiratory Infections Including SARS-CoV-2 through Promoting Metabolic and Immune Fitness with Probiotics and Plant Bioactives. Shinde T, Hansbro PM, Sohal SS, Dingle P, Eri R, Stanley R. Microorganisms. 2020 Jun 18;8(6):921. doi: 10.3390/microorganisms8060921. PMID: 32570850
Aging (Albany NY) . 2020 May 29;12(10):9959-9981. doi: 10.18632/aging.103344. Epub 2020 May 29. Why Does COVID-19 Disproportionately Affect Older People? Amber L Mueller 1 , Maeve S McNamara 1 , David A Sinclair 1 PMID: 32470948 PMCID: PMC7288963 DOI: 10.18632/aging.103344
Int J Mol Sci. 2019 Sep; 20(18): 4472. Published online 2019 Sep 10. doi: 10.3390/ijms20184472 Inflammaging and Oxidative Stress in Human Diseases: From Molecular Mechanisms to Novel Treatments Li Zuo,1,2,3,* Evan R. Prather,2 Mykola Stetskiv,2 Davis E. Garrison,2 James R. Meade,2 Timotheus I. Peace,1 and Tingyang Zhou2,3
Gastroenterology . 2020 May 19;S0016-5085(20)34701-6. doi: 10.1053/j.gastro.2020.05.048. Online ahead of print. Alterations in Gut Microbiota of Patients With COVID-19 During Time of Hospitalization Tao Zuo 1 , Fen Zhang 1 , Grace C Y Lui 2 , Yun Kit Yeoh 3 , Amy Y L Li 4 , Hui Zhan 1 , Yating Wan 1 , Arthur Chung 1 , Chun Peng Cheung 1 , Nan Chen 1 , Christopher K C Lai 5 , Zigui Chen 5 , Eugene Y K Tso 6 , Kitty S C Fung 7 , Veronica Chan 6 , Lowell Ling 8 , Gavin Joynt 8 , David S C Hui 2 , Francis K L Chan 9 , Paul K S Chan 10 , Siew C Ng 11 PMCID: PMC7237927 DOI: 10.1053/j.gastro.2020.05.048
ASSESSING THE AGE SPECIFICITY OF INFECTION FATALITY RATES FOR COVID-19: SYSTEMATIC REVIEW, META-ANALYSIS, AND PUBLIC POLICY IMPLICATIONS Andrew T Levin, Gideon Meyerowitz-Katz, Nana Owusu-Boaitey, Kensington B. Cochran, Seamus P. Walsh. doi: https://doi.org/10.1101/2020.07.23.20160895
Most of the studies I mention here are put up on our Natural Health, Healing and Remedies facebook page https://www.facebook.com/groups/607774773036636